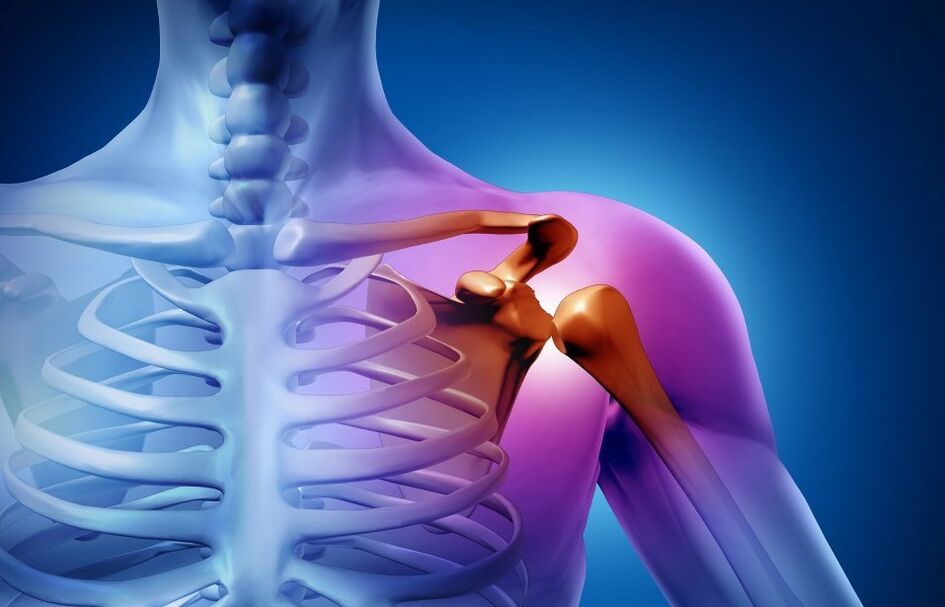
Osteoarthritis of the shoulder joint (joint) is a chronic disease in which irreversible degenerative-dystrophic processes occur in the tissues of the joint. The pathology disrupts the normal function of the limb. The range of motion of the shoulder is gradually reduced to complete immobility. Osteoarthritis of the shoulder joint causes severe pain and reduces the quality of life. In the absence of treatment, disability occurs.
To stop the processes of joint destruction and to maintain the mobility of the shoulder joint, it is necessary to contact an orthopedic traumatologist after the onset of the first symptoms.
Causes of osteoarthritis of the shoulder joint
The disease is multifaceted. The development of deforming arthropathy of the shoulder joint can be associated with several factors:
- Professional sports or intense training.
- Endocrine diseases.
- Hormonal disorders.
- Congenital pathologies of the development of the musculoskeletal system.
- Hereditary predisposition etc.
In most cases, secondary arthropathy is diagnosed: the pathology occurs after exposure to the joint of one or another factor. The primary or idiopathic form of the disease is rarely recorded. It is impossible to determine the exact cause of tissue degeneration in this case.
Symptoms of osteoarthritis of the shoulder
Changes in cartilage and bone tissue begin long before the first signs of arthritis appear. Articular structures have great potential for self-healing, so pathologies are rarely diagnosed at a young age, when all metabolic processes are quite active. As the body ages, recovery processes give way to degeneration. The first signs of destruction may appear after 40-50 years and with a deforming type of disease, patients notice changes as early as 16-18 years.
Symptoms of shoulder osteoarthritis:
- Cracking of the joint during movement.
- Pain, especially intense after exercise.
- Movement stiffness, expressed after sleep or long rest.
- Increased pain during weather changes.
Degrees of arthritis
The clinical classification defines three degrees of articulation of the shoulder joint:
- 1 point. The patient complains of a slight crease that occurs during movement. The pain syndrome is absent. The discomfort is felt when the hand is moved to the extreme position.
- 2 points. The pain occurs when the limb is raised above shoulder level. The range of motion is reduced. After considerable effort, the patient feels pain even at rest.
- 3 degrees. Joint mobility is severely limited. The pain syndrome is almost constant.
Diagnosis of osteoarthritis of the shoulder joint
The doctor not only needs to correctly diagnose, but also to determine the cause of the pathology. Treatment of the underlying disease significantly improves the patient's well-being and slows down cartilage degeneration.
Manual examination
The first stage of diagnosis is a consultation with an orthopedic traumatologist. The doctor examines the affected joint for swelling, severe deformity. On the development side of arthropathy, the muscles may partially atrophy - this can be seen with the naked eye.
With a manual examination, the doctor evaluates the function of the joint according to various criteria:
- Ability to voluntary hand movements.
- Thickening of the edges of the articular surfaces (large osteophytes can be detected by palpation).
- The presence of creases, "clicks" that are heard or felt by hand during shoulder movement.
- Blockage of the joint in the presence of free cartilage bodies.
- Pathological movements in the shoulder.
X-ray
To detect signs of arthropathy of the shoulder joint, the x-ray is performed in two views, which allows you to assess the degree of narrowing of the joint space, the condition of the bone surfaces, the size and number of osteophytes, the presence of fluid. and inflammation of the surrounding tissues.
Ultrasound (ultrasound)
A non-invasive method that allows you to examine the joints in pregnant and young children. According to the ultrasound, the doctor determines the thickness of the cartilage, the condition of the synovial membrane. The method visualizes well the osteophytes, the enlarged lymph nodes in the periarticular space.
Magnetic resonance imaging (MRI)
The MRI machine takes pictures of successive sections. The images clearly show not only the joint, but also the adjacent tissues. To date, MRI is one of the most informative methods in the diagnosis of joint pain.
Laboratory Tests
In the context of a comprehensive examination, they define:
- General blood test. Based on the results, the doctor can judge the presence and severity of the inflammatory process. The analysis also helps to assess the general state of health.
- Urine analysis. Kidney pathologies often cause secondary deforming arthropathy. Analysis is necessary for an accurate diagnosis.
- Blood chemistry. The data help determine the cause of inflammation. Biochemical analyzes are also performed to monitor complications and side effects during treatment.
Treatment of osteoarthritis of the shoulder joint
The treatment is long and difficult. The course of treatment includes medication, wellness procedures, a set of special exercises for arthritis of the shoulder joint. In difficult cases, surgery is indicated.
Medical treatment
Medications and dosage are selected separately. Your doctor may prescribe:
- Non-steroidal anti-inflammatory drugs (NSAIDs). Medications reduce inflammation and pain.
- Glucocorticosteroid preparations. Hormone-based media have a more pronounced effect on the focus of pain. Drugs not only relieve the patient's condition, but also reduce inflammation, have antihistamine and immunosuppressive properties. Glucocorticosteroids are prescribed in cases where NSAIDs are not effective.
- Painkillers. Drugs in this group are prescribed for severe pain syndrome. Depending on the severity of the symptoms, the doctor chooses non-narcotic or narcotic (rare) analgesics.
- Chondroprotective. The active ingredients of the drugs are involved in the formation of new cartilage tissue. The regeneration of the diseased joint is accelerated, nutrition is improved. Chondroprotectants have a cumulative effect and have been shown to treat arthritis of varying severity.
Some drugs are injected directly into the joint cavity. For example, blockade has a better analgesic effect than taking tablets.
Physiotherapy
The lessons are held after the removal of the flare. Physiotherapy as part of the combination therapy helps to improve the delivery of drugs to the affected joint, relieve swelling and reduce pain.
For the treatment of the joint use:
- Electrophoresis.
- Phonophoresis.
- Shock wave therapy.
Physiotherapy can be combined with massage, gymnastics, therapeutic baths. It is best to undergo a set of procedures based on a specialist clinic. The doctor will make a treatment plan taking into account the condition of a particular patient.
Physiotherapy
Moderate physical activity is important for slowing down degenerative processes. It is best to start exercise therapy for arthritis of the shoulder at a medical center, under the supervision of a doctor. The specialist will select the exercises, teach them how to perform them correctly and distribute the load so as not to cause an exacerbation of the disease. Exercise usually includes warm-ups, stretching and strength training. Exercises are performed at least 3 times a week.
After a course with a specialist, patients can perform therapeutic exercises for arthritis of the shoulder joint at home.
Surgery
The operation is performed with grade 3 arthropathy, when the disease no longer allows the patient to move normally, it causes severe pain and the prescribed treatment does not help.
There are several methods of surgical treatment:
- Puncture. A long needle is inserted into the joint cavity and the accumulated fluid is pumped out. The puncture reduces the pressure, reduces the swelling, increases the mobility of the joints. The procedure is minimally invasive, so it is performed in outpatient clinics. Material obtained during the puncture is sent for investigation to determine the infectious agent or other markers.
- Arthroscopy. With the help of microsurgery tools, the doctor examines the joint cavity, removes scar tissue, sutures the rotator cuff tendons or the joint, if they are damaged. Several punctures remain in the skin. The patient recovers quickly.
- Endoprosthesis. The endoprosthesis allows you to completely get rid of the chronic pain, to restore the mobility of the arm. After the operation, long (from 3 to 6 months) rehabilitation is needed.

















































